A first-of-its-kind symposium held last month at Memorial Sloan Kettering brought together scientists from across the globe to discuss a promising new cancer treatment called CAR T cell therapy.
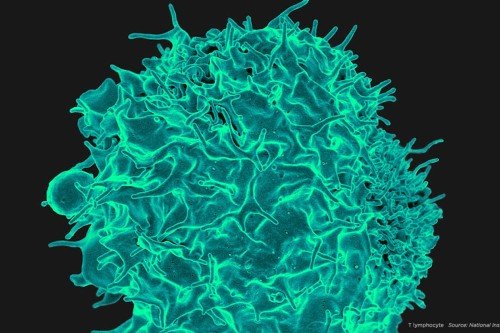
CAR stands for chimeric antigen receptor. A type of immunotherapy, CAR T cell therapy involves removing immune cells from a patient, arming them with proteins that recognize cancer targets, then giving them back to the patient in vast numbers.
This approach has demonstrated remarkable results in patients with chemotherapy-resistant leukemia, and is now being explored as a treatment for several other types of cancer.
Hundreds of scientists attended the event, which was organized as a continuing medical education course by Prasad S. Adusumilli, Deputy Chief of MSK’s Thoracic Surgery Service and a member of the Center for Cell Engineering and Center for Cellular Therapeutics at MSK. Michel Sadelain, a pioneer of CAR T cell therapy and Director of the Center for Cell Engineering, and Renier Brentjens, Director of Cellular Therapeutics at MSK, were co-directors of the course.
Like the larger field of immunotherapy, of which it is a part, CAR T cell therapy has progressed rapidly in a short time. In his opening remarks, MSK Physician-in-Chief José Baselga expressed great optimism about the approach. “It’s hard for me to visualize a field that has more promise than cellular therapy in cancer,” he said. “What’s happening today is just short of a miracle for many of us.”
Getting to the Starting Line
In 32 presentations and two keynote addresses, participants explored the current status of CAR clinical trials, effective management of patients receiving this treatment, and new developments in CAR technology. They also looked back at the evolution of the field.
In his keynote, Zelig Eshhar, of the Weizmann Institute in Israel, discussed research on immune cell receptors he conducted in the late 1980s and early 1990s, which helped pave the way for current CAR technology.
Dr. Eshhar showed that it was possible to splice together the genetic information from two different immune molecules into a single gene. The hybrid gene could then be transferred into a T cell, which would make the gene product — a chimeric receptor on the cell surface.
In terms of efficacy, the first generation of CARs were essentially clunkers. They did not have the hoped-for efficacy at fighting cancer. Nevertheless, researchers were intrigued by the possibilities.
In his keynote address, Dr. Sadelain, who had engineered T cells at the Massachusetts Institute of Technology in the late 1980s before joining MSK, described how he identified problems in the early CAR T cell design.
It turns out that engineered T cells need more than just an activation signal to sustain their therapeutic activity; they also need a “co-stimulatory” signal. One of Dr. Sadelain’s major contributions to the field was to create a CAR with activation and co-stimulatory molecules fused together. He called these “second-generation CARs.” He and his colleagues, including Isabelle Rivière and Dr. Brentjens, then worked together to translate these CARs to the clinic.
Back to topSuccessfully Test-Driving CARs
CAR T cell therapy has had the most dramatic success in treating acute lymphoblastic leukemia (ALL), a type of blood cancer that affects white blood cells called B cells.
All B cells — both cancerous and normal — make a protein called CD19. It was Dr. Sadelain’s perceptive idea back in 1994 to focus on CD19 as a target for CAR therapy.
Clinical results using CD19-targeted CARs have been impressive. At MSK, 37 out of 46 ALL patients (82%) who were treated with CAR T cell therapy experienced a complete response. Some of these patients went on to have a stem cell transplant, and many remain free of cancer today.
At MSK, there are currently eight open clinical trials testing CAR T cell therapy in six different cancer types — leukemia, lymphoma, mesothelioma, lung, breast, and ovarian cancer. These trials are made possible through the support of the Cell Therapy and Cell Engineering Facility, led by Dr. Rivière, which manufactures the T cells for these patients.
During his talk, Dr. Brentjens discussed how MSK established procedures for uniform clinical trial preparation, protocol development, and patient management algorithms with multidisciplinary participation across the institution.
Back to topNext-Generation CARs
In addition to CD19, researchers are steering CARs at other potential cancer targets, including cancer-associated proteins such as HER2, EGFR, MUC1, and mesothelin. This last example represents an attractive target for cancers such as mesothelioma, non-small cell lung, triple-negative breast, ovarian, and pancreatic cancers, which make the protein in abundance.
Several researchers discussed their efforts to engineer CARs that can also produce drugs — so-called “armored CARs.” This approach is currently being tested in a clinical trial at MSK for the treatment of relapsed ovarian cancer.
As a type of solid tumor, ovarian cancer represents the next frontier for CAR T cell therapy. Solid tumors have so far been less responsive to this form of treatment. The armored CARs being directed at ovarian cancer produce an immune molecule called IL-12, which boosts immune responses. Dr. Adusumilli discussed a novel clinical trial in which CAR T cells are directly delivered to the tumor bed, which has shown higher efficacy in preclinical studies.
Another tactic to give CARs more oomph is to combine them with immune drugs called checkpoint inhibitors, which “release the brakes” on immune cells. Like regular T cells, CAR T cells have braking molecules, such as PD-1, that can reduce their efficacy. Dr. Adusumilli is conducting laboratory studies of CAR T cell therapy in combination with an anti–PD-1 drug. He is also the principal investigator of a trial of mesothelin-targeted CARs for mesothelioma, lung, and breast cancers.
Back to topBeyond Tumor Targeting
In his keynote, Dr. Sadelain made clear that CARs might one day find uses beyond tumor cell killing. They might be used to reprogram the “tumor microenvironment,” he says, serving as a kind of vaccine in addition to directly eliminating tumor cells. Or they could be used to fight infectious and autoimmune diseases. Even regenerative medicine — repairing organs from the inside out — might benefit.
“CARs are making history, beyond any doubt,” Dr. Sadelain said.
Invited faculty: Steven M. Albelda, MD, University of Pennsylvania; Christine Brown, PhD, City of Hope; Laurence J. N. Cooper, MD, PhD, MD Anderson; Marco L. Davila, MD, PhD, Moffitt Cancer Center; Soldano Ferrone, MD, PhD, Massachusetts General Hospital; Noelle Frey, MD, MSCE, University of Pennsylvania; Rebecca A. Gardner, MD, Seattle Children’s Hospital; Adrian P. Gee, PhD, Baylor Medical Center; David Gilham, PhD, University of Manchester; Stephen Gottschalk, MD, Baylor Medical Center; Michael C. V. Jensen, MD, Seattle Children’s Hospital; James N. Kochenderfer, MD, National Cancer Institute; Daniel W. Lee, MD, National Cancer Institute; Bruce L. Levine, PhD, University of Pennsylvania; John Maher, PhD, FRCPath, King’s College London; Shannon L. Maude, MD, PhD, Children’s Hospital of Philadelphia; Marcela V. Maus, MD, PhD, Massachusetts General Hospital; David L. Porter, MD, University of Pennsylvania; Stephen J. Schuster, MD, University of Pennsylvania; Cameron J. Turtle, MD, PhD, Fred Hutchinson Cancer Center
MSK faculty: Kevin J. Curran, MD, Pediatrics; Sergio A. Giralt, MD, Chief, Bone Marrow Transplant; Roisin E. O’Cearbhaill, MD, Gynecologic Medicine; Jae Park, MD, Leukemia; Isabelle Riviere, PhD, Cell Therapy & Cell Engineering; Paul Sabbatini, MD, Deputy Physician-in-Chief; Craig S. Sauter, MD, Bone Marrow Transplant; David A. Scheinberg, MD, PhD, Chair, Molecular Pharmacology Program; Marcel R.M. van den Brink, MD, PhD, Division Head, Hematologic Oncology – Medicine; Roger S. Wilson, MD, Institutional Review Board; Jedd D. Wolchok, MD, PhD, Chief, Melanoma & Immunotherapeutics; Renier J. Brentjens, MD, PhD, Director, Center for Cellular Therapeutics; Prasad S. Adusumilli, MD, FACS, FCCP, Member, Center for Cell Engineering & Center for Cellular Therapeutics, Deputy Chief, Thoracic Surgery Service; Michel Sadelain, MD, PhD, Director, Center for Cell Engineering
Back to top