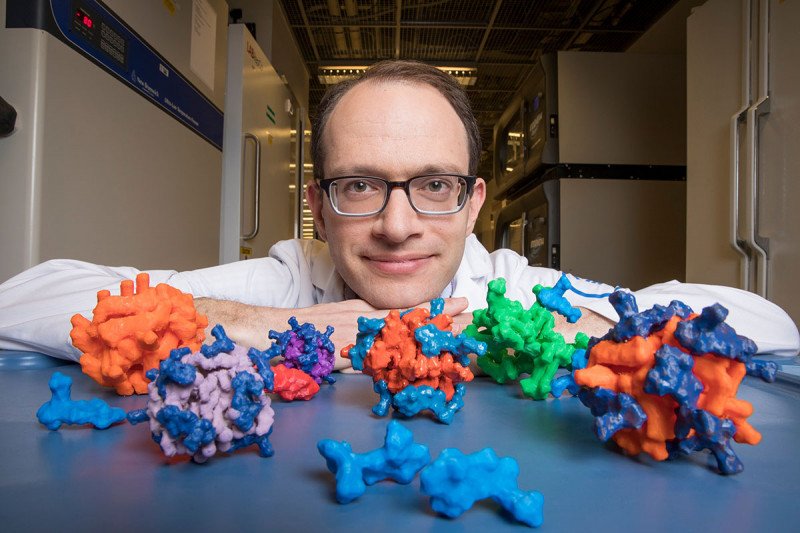
Particle Man: Chemist Daniel Heller with 3-D-printed models of his cancer-fighting nanoparticles.
In cancer treatment, as in fashion, one size rarely fits all. The goal of personalized cancer medicine is to tailor a treatment to the specific genetic makeup of a cancer. Drugs that target a tumor’s unique genetic weaknesses have become an important part of modern cancer care.
Yet even personalized medicines can have unwanted side effects. In part, this is because they travel to many healthy tissues in the body, not just to the tumor. A new approach devised by nanotechnology experts at the Sloan Kettering Institute (SKI) may make personalized medicines more precise by helping them avoid collateral damage.
“We found a way to use machine-learning algorithms to design powerful nanomedicines that can deliver a stronger, safer, more personalized punch,” says Daniel Heller, a chemist in the molecular pharmacology program at SKI and an assistant professor at the Weill Cornell Graduate School of Medical Sciences. Dr. Heller’s laboratory specializes in designing nanotechnologies that improve the detection and treatment of cancer.
The computer-aided method allows nearly any class of personalized drug to be packaged into a nanoparticle. The approach could help make these drugs both safer and more effective.
Nanoparticles are tiny objects with diameters less than one-thousandth of a human hair. Scientists have previously used nanoparticles to deliver drugs in the body. But so far it’s been difficult to design them to carry the newer types of cancer medicines.
“Machine learning has been enlisted to do amazing things for us, like steer a self-driving car or help scientists find patterns in large amounts of human genome data,” Dr. Heller says. “So we thought it might help us design better nanomedicines.”
Using Chemical Structures to Make Predictions about Nanoparticles
Dr. Heller and a postdoctoral fellow in his lab, Yosi Shamay, started from the observation that some drugs easily assemble into nanoparticles while others do not. They wondered if they could work backwards from this result to determine what qualities about a drug can influence its ability to form a particle. They used machine-learning algorithms to churn through many, many types of data to come up with the common elements of good particle makers.
“It turned out that we could predict with remarkable accuracy whether a particle would form or not based on the structure of the drug,” Dr. Shamay says. He notes that they can also run the method backwards and use it to determine how to design a drug molecule so that it will form a nanoparticle.
These new nanoparticles are different from their predecessors in an important way. Previous versions mostly consist of a polymer that acts like a glue holding the particle together. The new particles are up to 90% drug, so they pack more of a wallop.
Back to topHelping Cancer Drugs Hit Their Molecular Mark
The SKI scientists demonstrated the effectiveness of their nanoparticles using drugs called MEK inhibitors. These personalized medicines are an effective treatment for certain types of cancer, including pancreatic cancer and lung cancer, which share certain mutations. But MEK inhibitors can also harm the normal cells in the skin. They can cause a severe rash, which can limit the amount of the drugs that can be given to people with cancer.
In mouse models of cancer, the MEK inhibitors packaged into nanoparticles hit their target without damaging the skin.
“If we target these new drugs directly to the tumors and away from the normal tissues, they will work a lot better, and the side effects would not be so bad,” Dr. Heller says. “That’s what we hope this nanotechnology will enable.”
This work was developed in collaboration with the laboratories of SKI researchers John Chodera, a computational chemist, and Scott Lowe, a cancer biologist. A paper describing the new findings appears in the journal Nature Materials.
Back to top




