There is an exciting new movement in cancer research — often referred to as exceptional responder investigation — that appears to be transforming past disappointments into progress. Here, we discuss how this approach can resurrect therapies whose development was previously halted.
The history of oncology is full of “unique cases” — anecdotes doctors tell one another about the single patient who had an impressive response to a treatment that failed many others. Until recently, these puzzling phenomena usually didn’t get much attention, since there was no way of telling why a therapy helped certain people but not others.
If, for example, a new drug tested in a clinical trial worked remarkably well for one patient and ten others got no benefit, the therapy traditionally would have been written off as ineffective. And most likely the doctors who led the trial would have moved on to investigate another drug instead.
But in the past couple of years, researchers have been returning to failed trials to dust off data about those few exceptional responders. And increasingly, they are able to solve these mysteries thanks to powerful new sequencing technologies that make it possible to inspect the DNA of these patients’ tumors and find out what makes their cancers unique.
The goal of this research is to make patients’ successful responses to investigational drugs the norm, or closer to it, rather than the exception. If scientists are able to show that a particular gene mutation is making one person’s tumor vulnerable to a drug, and there’s a plausible explanation for why the drug is working, other patients with the same mutation — even in a different type of cancer — have a fair chance of benefiting from the treatment as well. Sometimes these patients can be offered the therapy in the context of a clinical trial.
A Breakthrough in Bladder Cancer
“Excitingly, many of these patients [with the same genetic mutations] are similarly responsive to the same therapy that was so effective in the outlier patient,” MSK clinician-scientist David Solit, who directs the Marie-Josée and Henry R. Kravis Center for Molecular Oncology (CMO), noted in a recent interview on this blog. “The approach has enabled us to resurrect therapies whose development was previously halted.”
In 2012, Dr. Solit and his co-workers published a groundbreaking study of a patient with advanced bladder cancer who participated in a clinical trial of a drug called everolimus (Afinitor®) and responded surprisingly well. The researchers decided to survey this patient’s disease in depth by sequencing the entire genome of her tumor. An examination of other patients on the trial showed that only those with TSC1 mutations in their tumors benefited from the drug.
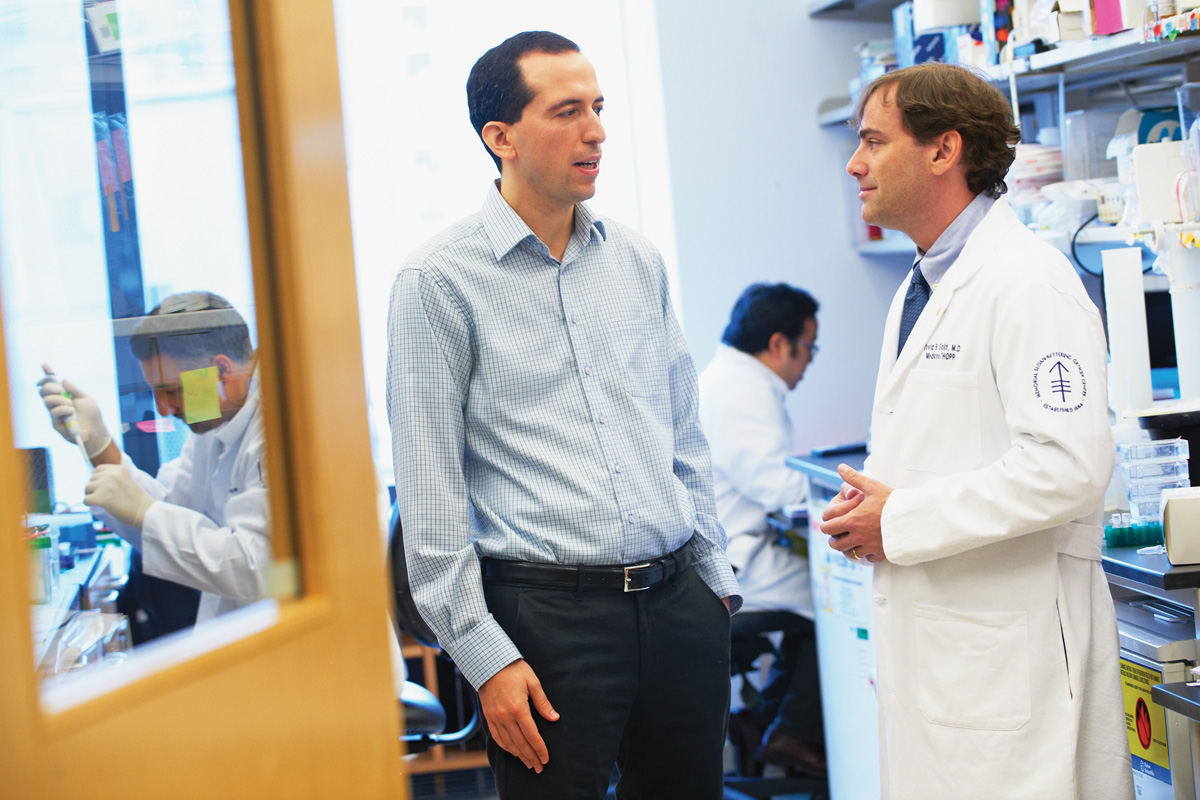
Cancer genomics researchers Michael Berger (left) and David Solit. Dr. Berger led the development of a tumor sequencing test that is used to guide treatment choices and identify patients who are candidates for basket trials.
Following this research, MSK scientists have conducted a number of similar investigations to identify extraordinary responders with different types of cancer with the goal of extending the treatments that helped them to other patients who might benefit. The bladder cancer study led by Dr. Solit also led the National Cancer Institute to launch the Exceptional Responder Initiative, a comprehensive effort to analyze the cancer genomes of up to 300 exceptional responders.
Back to topBasket Studies
MSK doctors are also pioneering a new way to conduct clinical trials — called basket trials — to more quickly test promising precision treatments. Traditional clinical trials enroll patients according to a particular cancer type. Basket trials, on the other hand, are designed around gene changes and so may be open to patients with different tumor types. They have been particularly impactful for patients with rare cancer types for whom few clinical trial options have previously existed.
Research on exceptional responders can help identify small subgroups of patients diagnosed with different cancers — breast, lung, bladder, and endometrial cancer, for example — who are likely to benefit from a specific treatment because their tumors have the same rare mutation. “Opening up separate trials for each type of cancer is often not feasible and would take years,” Dr. Solit says. “Instead, we conduct one study in which patients with any of these cancers can enroll.” Researchers at MSK have initiated an increasing number of these basket trials in recent years.
A new type of clinical trial called a basket trial can speed the development of precision treatments.
Since last year, our pathologists have been analyzing the tumor DNA of essentially all MSK patients with advanced cancer using a new genomic sequencing test developed by MSK scientists. This routine testing allows doctors to detect clinically “actionable” tumor mutations that can help inform treatment choices — or, in some cases, identify patients who are candidates for a basket trial.
There are good indications that the approach is paying off. A recent study that explored the value of genomic testing for guiding lung cancer treatment showed that in two-thirds of patients, tumor sequencing led to the identification of actionable mutations. And those patients who were able to receive a therapy matched to their specific mutation had better outcomes than patients receiving standard treatment.
On March 26, MSK medical oncologist David Hyman was on WNYC’s Morning Edition to talk about a brain tumor patient who benefited from a drug originally tested for skin cancer. Learn more and listen to the program.
Back to top