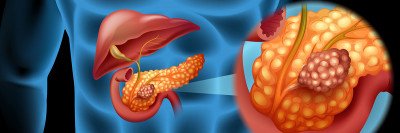
The pancreas (orange) is a small digestive organ located near the stomach. Pancreatic tumors are hard to detect early and are not easily treated with surgery or chemotherapy once they spread to other organs.
Just 7% of people with pancreatic cancer are alive after five years. The pancreatic cancer survival rate after ten years is less than 2%.
Yet among these dismal statistics is a faint glimmer of hope. Some people with pancreatic cancer manage to beat the odds, surviving for many years after their initial diagnosis — maybe even long enough for doctors to use the word “cure.”
“Nobody knows why these patients live longer than other people with pancreatic cancer,” says Vinod Balachandran, a surgeon-scientist affiliated with the David M. Rubenstein Center for Pancreatic Cancer Research and a member of the Parker Institute for Cancer Immunotherapy at Memorial Sloan Kettering who specializes in the disease. “But something is clearly setting them apart.”
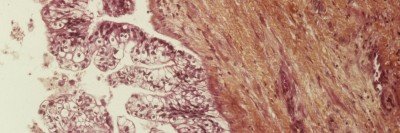
In a study, he and his colleagues set out to identify what that something is. Suspecting that the immune system might be involved, they looked at the number of immune cells present in a tumor and found the more immune cells, the longer the survival.
What’s more, they were able to identify the particular components of the tumor that drew those immune cells in. The results, reported in the journal Nature, have implications for the design of more-effective immunotherapies for people with all types of cancer, including the deadly pancreatic cancer.
Uncloak and Dagger
Dr. Balachandran and his colleagues, including Jedd Wolchok, Timothy Chan, Steven Leach, and Taha Merghoub, looked at patients whose pancreatic tumors were surgically removed and who in some cases received subsequent chemotherapy. Compared with pancreatic tumors from people who had low survival rates, tumors from long-term survivors (average survival of six years) had nearly 12 times the number of immune cells called T cells inside them. The presence of many T cells meant a better pancreatic cancer prognosis.
T cells are specialized at distinguishing foreign invaders, like infections and cancer, from normal body cells. They recognize bits of proteins on the cells’ surface called antigens, which serve as a kind of molecular fingerprint.
Dr. Balachandran and his team took a closer look at the antigens found in the tumors. They focused on a subset of these called neoantigens, which cancer cells accumulate as a result of mutations when they divide. The group discovered that tumors of long-term survivors contained particularly good neoantigens — ones that T cells could recognize as foreign. As Dr. Balachandran explains, these neoantigens may have, in effect, uncloaked the tumors to T cells, allowing T cells to attack and kill them.
Even more striking, T cells recognizing these neoantigens were present in the blood of long-term survivors up to 12 years after the tumors had been removed by surgery. This result suggests that the immune system in these people had generated long-lasting “memory” of the cancer and was keeping it in check. “We think that these long-term survivors highlight how neoantigens can be used in generating long-lasting immune responses against tumors,” Dr. Balachandran says.
An advantage of the study was its relatively large size. “Before our work, the largest study looking at long-term survivors of pancreatic cancer had only eight patients,” Dr. Balachandran says. “We had 82.”
To further define what makes a good neoantigen, the MSK team joined up with computational biologists Benjamin Greenbaum and Marta Luksza from the Icahn School of Medicine at Mount Sinai. They built an algorithm to predict the best neoantigens out of the many possible ones. These results were reported in a separate article, also published in Nature.
Back to topBoosting Immune Responses
Knowing what the immune system is seeing in particular tumors opens the door to therapeutic approaches geared toward deliberately focusing on these targets. For example, doctors could make a therapeutic cancer vaccine composed of several distinctive neoantigens identified from a patient’s own tumor. A form of personalized immunotherapy, this type of vaccine would help boost the immune system against those targets that are most likely to generate an effective and lasting immune response. Recent reports have demonstrated the feasibility of this approach in people with other cancers.
Is pancreatic cancer curable? The answer is a long way off, but immunotherapy will likely play an important role if this goal is achieved.
“We think our findings are a step forward in being able to predict rationally which neoantigens will be the most effective at stimulating an immune response,” he says. “We envision using these results to design more effective cancer vaccines to be used in combination with other immune therapies.”
The team is now engaging with the pharmaceutical companies Genentech and BioNTech to determine how to use these insights in clinical trials evaluating personalized neoantigen vaccines in a spectrum of cancers, including pancreatic cancer and melanoma. “We are determined to move this forward to clinical trials as quickly as possible,” Dr. Balachandran says.
Back to top